Understanding the true cost of clinical trials
Written by Alicia Staley, chief patient officer, Medidata
Estimated reading time: 8 minutes


Clinical development in rare disease is inherently a high-risk and resource-intensive endeavour. Yet despite decades of investment, trial performance metrics remain concerning at best: 30% of patients drop out of trials, and over 85% fail to recruit on time1. These statistics are not mere inefficiencies; they represent systemic misalignment between trial design and patient realities. The result is delayed therapies, lost time and significant capital waste.
Reviewing the quantifiable cost of clinical trial delays in the rare disease community can help build the case for a strategic investment in the patient experience as the foundation to address drug development risk, improve operational efficiency and increase return on investment. This objective can be achieved with the shared goal of patient centric trial delivery.
Rare disease trials face distinct barriers: limited patient pools, complex care regimens and higher operational costs. According to Tufts CSDD, for each month a clinical trial is delayed, the trial team can incur costs between $600,000 and $8 million2. In rare disease clinical trials, the stakes are even higher. Recruitment delays or dropout-related data attrition can jeopardise entire programmes, especially in smaller biotech portfolios.
Recent data shows that 30% of Phase III rare disease studies are unsuccessful due to enrolment challenges3. In addition, more than 50% of rare diseases impact children, adding layers of complexity to protocol design, consent and logistics.
Taken in context, the outcome is distressing. Only 1 in 4 rare disease drugs that get through Phase I trials make it to market4. This reduced success rate is not solely due to therapeutic inefficacy. These trials often fail because the operational model neglects the patient experience.
Sponsors face multiple downstream costs when a trial is unsuccessful or underperforms. Consider the following:
- Protocol amendments: Affect over 60% of trials with a median cost of $500,000 per amendment5.
- Ongoing recruitment cycles/waves: When screen failures and dropout rates exceed the original forecast and plans, additional resources are needed to keep the trial in “perpetual recruitment.”
- Regulatory delays: When trials deal with data quality issues due to lower data collection (total volume).
While clinical risk is inherent in R&D, many operational failures are preventable. Patient experience, when treated as a strategic asset, offers a path to mitigation.
Integrating the patient perspective into trial design and operations delivers tangible financial and performance outcomes. A study from McKinsey & Company shows that trials co-designed with patients enrol up to 60% faster6. Understanding the lived experience, particularly in the rare disease communities, can shed light on potential issues and roadblocks that impact a trial’s success. By identifying and addressing patient burden upfront, trial teams can better support the end-to-end patient experience. Patients can help identify key support and infrastructure needed to shape the patient experience and can deliver up to 25–30% higher engagement and retention in trials7. Higher adherence and fewer amendments increase the probability of trial success, leading to improved protocol feasibility and savings of $2–5 million per trial8.
Ultimately, this up-front, early investment pays off later in the trial during regulatory review. Trials that reflect real-world patient data and needs are more likely to achieve endpoints that regulators consider clinically meaningful.

At Medidata, we view patient experience as a cross-functional responsibility that impacts the entire software development life cycle. Our Patient Insights Board is a group of patients, caregivers, and advocates who are experts in their lived condition. They have in-depth knowledge of the clinical trial ecosystem and help us create better solutions to address key challenges facing the industry. Through our Patient Insights Board, we consistently receive feedback from our patient advocates about the trial experience. Some key findings they’ve shared:
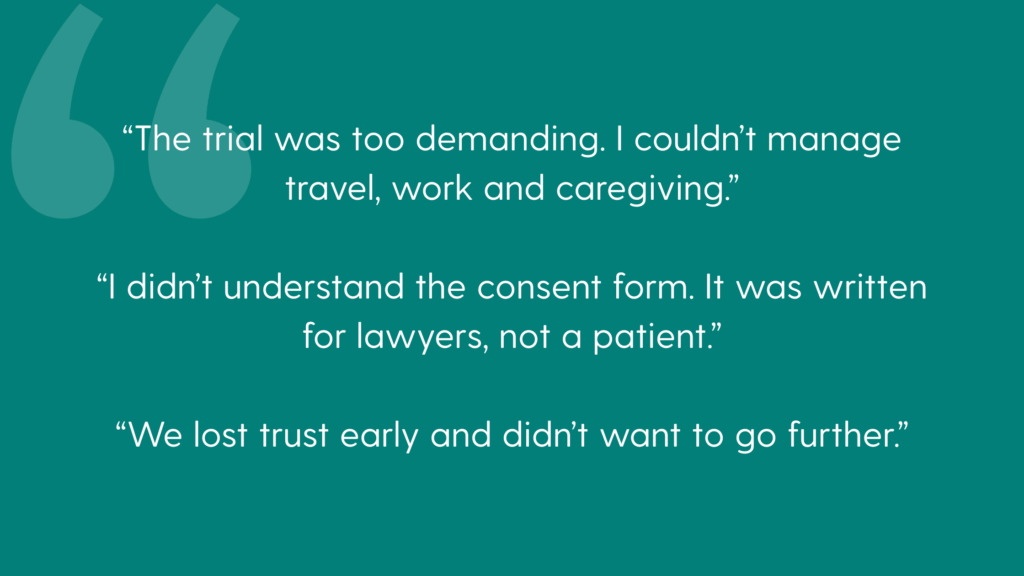
These are not anecdotes. They are indicators of design failure. Sponsors that ignore the patient perspective not only risk trial failure but brand erosion in small, but vocal patient communities.
Trust is a currency in clinical trials and to lose the patient communities is to lose access and feedback necessary for success. Trials succeed not because insights change the science, but because they change the patient experience.
Rare disease non-profits play an indispensable role as trusted intermediaries in clinical research and patient advocacy. Their early and sustained involvement is critical for several reasons, primarily de-risking patient recruitment and significantly enhancing the credibility of clinical studies.
These organisations often possess deep, intrinsic knowledge of the specific rare disease communities they serve. They understand the nuances of patient needs, the challenges of diagnosis and the complexities of living with a rare condition. This intimate understanding allows them to bridge the gap between researchers and patients, fostering a sense of trust and collaboration that is often lacking in more traditional recruitment models.
By engaging rare disease non-profits from the outset of a study’s design, sponsors and researchers can tap into established networks of patients, caregivers and medical professionals who are actively engaged with the disease. This connectivity not only streamlines the identification of eligible participants but also helps to overcome common barriers to enrolment, such as geographical dispersion of patients or lack of awareness about clinical trials. The non-profits can effectively disseminate information about studies, answer patient questions in a culturally sensitive manner and provide the necessary support to encourage participation.
The endorsement and active involvement of a respected rare disease non-profit lend significant credibility to a clinical study. Patients and their families are more likely to trust a study that is championed by an organisation they already rely on for information, support and advocacy. This enhanced credibility can lead to higher recruitment rates, greater patient retention and ultimately, more robust and reliable study outcomes. Their involvement also often ensures that the study design is patient-centric, considering the unique burdens and perspectives of those living with the rare disease, thereby making the research more relevant and impactful.
To improve performance in rare disease clinical development, organisations should:
- Build protocols from the patient journey outward: Start by mapping the day-to-day realities of patients and caregivers. Incorporate insights from lived experience to ensure protocols are feasible, minimally disruptive and aligned with the participant motivations.
- Fund concierge and hybrid participation models: Provide support services such as travel coordination, telemedicine, at-home visits and caregiver stipends. These models reduce common barriers to participation and signal to families that their time and wellbeing are valued.
- Integrate non-profit partners from inception: Engage advocacy groups early in protocol design and recruitment planning. Their deep understanding of the community builds trust and accelerates enrollment while also improving the cultural relevance of materials and communications.
- Embed patient metrics into corporate performance: Incorporate patient-reported experience data, recruitment timelines and retention rates into organisational KPIs. This ensures that patient engagement is prioritised not just in rhetoric, but in operational and financial decision-making.
- Elevate patient leadership roles: Establish C-level roles like chief patient officer and ensure these leaders have both authority and resources to shape strategy. Their presence creates cross-functional accountability and ensures patient priorities are embedded across R&D, commercial and compliance functions.
When trials fail to recruit or retain, it’s not just a missed milestone—it’s a lost opportunity to change lives and recoup R&D investment. Rare disease trials are too complex, costly, and vital to be designed without the input of those they intend to serve.
The evidence is clear: patient-centered trials are faster, cheaper, and more likely to succeed. The tools, models, and data already exist. What’s needed now is broader adoption and leadership commitment.
Families impacted by rare diseases cannot afford for us to get this wrong, and neither can the industry.
Alicia Staley is chief patient officer at Medidata, leading the Social Impact and Engagement teams to amplify patient, site and employee insights across the product lifecycle. A three-time cancer survivor, Alicia uses her personal experiences and empathy to champion patient-centric innovation.
With more than 25 years of experience in software design and information systems management, Alicia maintains an extensive network of patient advocates, non-profits and industry stakeholders organisations to enhance policies and practices to improve cancer care. As a champion of patient advocacy and engagement, Alicia understands the critical issues facing patients seeking to engage in clinical research.
Connect with Alicia
References
[1] CISCRP. 2019 Perceptions & Insights Study. Center for Information and Study on Clinical Research Participation.
[2] Getz, K. A. et al. The Impact of Protocol Amendments on Clinical Trial Performance and Cost. Tufts CSDD Impact Report. 2016.
[3] Clinical Leader. Rare Disease Patient Recruitment and Retention: Overcoming the Challenges.
[4] Wong CH, Siah KW, Lo AW. Estimation of clinical trial success rates and related parameters. Biostatistics. 2019
[5] Getz K, Smith Z, Kravet M. Protocol Design and Performance Benchmarks by Phase and by Oncology and Rare Disease Subgroups. Ther Innov Regul Sci. 2023 Jan
[6] McKinsey & Company. Patient-Centric Trials: Enrolling Faster and Retaining Longer. Life Sciences Practice. 2021.
[7] Deloitte. How to successfully launch a rare disease drug in a patient-centric world.
in the loop lets you stay informed with all the latest issues from the world of RARE. To access more in the loop articles click below.

