“The Great Democratisation”. How AI is levelling the playing field for patients

Written by Dr Michael Trueman, co-founder and CEO, Advoca Health
In a similar fashion to Tolkien’s Palantiri or Pullan’s Alethiometer, open access to advanced logical reasoning trained on the entirety of human knowledge has changed life for people all around the world, who now have super-human informational capabilities that have never been seen before (in the history of mankind).
Perhaps I am being superlative when I compare tools like ChatGPT and Gemini to mystical artefacts from fantasy literature, but the point stands. Artificial Intelligence (AI) presents the largest opportunity ever for ordinary people and communities in achieving super-ordinary outcomes for themselves and others. This is especially relevant in the context of health.
For centuries, information about health, wellness and disease was gate-kept by the lowest common denominator—literacy. In the Middle Ages you would be very fortunate to be one of the 5% of people who could read and write, and even more fortunate to have access to books containing any sort of information to help you cure your ailments.
Fortunately, in today’s day and age, the overwhelming majority of people in high income countries are literate and now have seamless access to context-intelligent software that retrieves information from every nook and cranny of the entirety of human knowledge. It is easy to see how things will be very different for you if you are a person seeking to learn about health and wellness in 2026.
The Shift:
Large Language Models (LLMs) underpin the functionality of many tools we now refer to as ‘AI’. At their core, LLMs are prediction models trained on vast amounts of text. They operate by predicting the most likely next word—or sequence of words—based on their analysis of the previous text in the passage, and the patterns of text they’ve been trained on. As a result, they can appear to follow reason and logic, but what they are actually doing is sophisticated pattern prediction, derived from their initial training data.
The great thing about LLMs is that they bring easy access to a lot of context derived information that could never otherwise be obtained quickly, which helps patients to get the information they require instantly, and in a greater depth and relevancy to their individual circumstances. Information can be tailored to your personal requirements. Furthermore, resources such as journal articles—often highly technical in nature—can be summarised and morphed into a format that is accessible to a lay person, replacing all of the technical jargon with easy-read text.
So, whilst LLMs are transformative (they really are great at communicating confidently with you!), it’s important to consider risk when applying them to niche contexts such as health, and especially rare diseases. An LLM’s training data on these specialist subsections of knowledge is incredibly small. The resultant output from questions relating to rare diseases is highly prone to hallucinations—phenomena defined as an output from an LLM that is delivered confidently, but factually incorrect or not based on its original training dataset. Practically, this introduces risk when seeking health advice, as there is a possibility that an LLM can hallucinate a health management suggestion that leads to no benefit, or worse, harm.
The same AI technology also gives huge opportunities for broader impact in the community, through analysis of people’s interactions with digital tools. Patient interactions with apps can be analysed to automatically generate a huge quantity of real-world evidence (RWE), with a granularity that has not been possible to achieve previously. Real world evidence is especially important in the context of rare disease as less is known about the lived impact of these conditions on patients, families and caregivers. A comprehensive RWE dataset is essential for evidencing community needs, advocating for change, and advancing new treatments swiftly into availability. The benefits of automating the generation of RWE for a nominal cost has the potential to be transformative for the care of people with rare diseases. In disease areas where research is difficult to fund, and current literature is few and far-between, patient engagement with the right digital tools that can perform this function has the potential to bring forth ground-breaking progress in rare disease R&D.
My co-founder Dr Shyam Dhokia and I set out on a mission to safely empower patients with AI across the entirety of the sector, whilst mitigating some of the key risks I’ve mentioned.
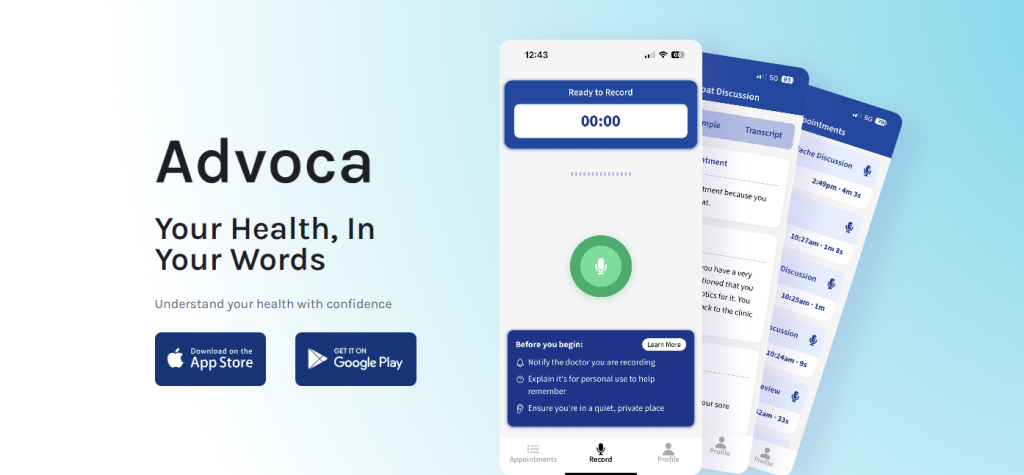
Over the course of 6-months we developed Advoca.
Advoca is a free mobile app that lets users safely record their appointments with healthcare professionals and then receive an accurate summary of everything discussed in patient-friendly language. This includes highlighting key points, results and agreed next steps. The result is a comprehensive post-appointment summary that can be referred back to over time by patients, families and caregivers.
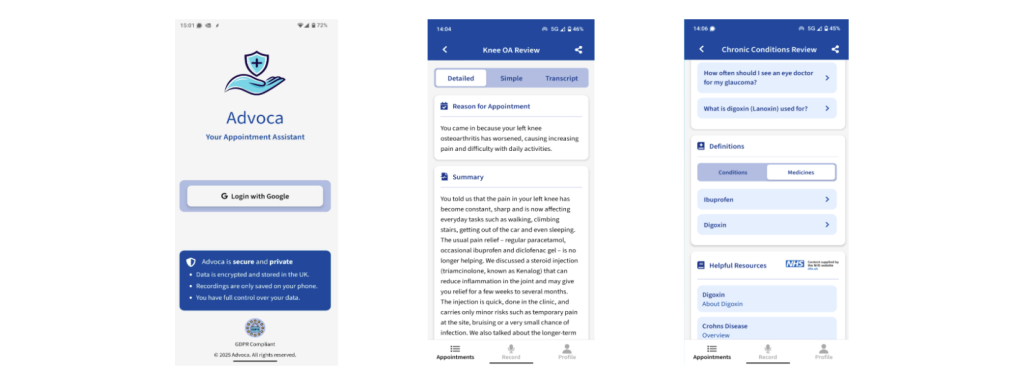
The presence of such a summary helps to improve confidence in one’s care and elevates the health literacy of the care recipient in their future interactions with clinicians. Advoca quickly becomes a helpful contribution to shared decision making between patients and their clinical team.
We then analyse the content and context of the conversation to signpost users directly to the best available online health resources for further reading. A significant component of patient-led management is influenced by one’s own research online. As such, we automate that process with direct signposting to safe and credible resources. This feature is contributed to by working alongside patient advocacy groups who know where the good resources are! As such, we successfully guide users to get a full suite of additional health resources, relevant to the discussion points in the appointment they have just attended.
This is a clear example of how AI can safely and effectively level the playing field for patients. By completely eliminating the attrition of knowledge that begins as soon as patients leave the clinic room, and translating it from medical jargon to ordinary words, a patient’s access to their own medical information is now higher than at any other point in history. This means that patients are now on greater parity with their clinical team, can make informed decisions and better advocate for their own medical needs and preferences.
When people with rare diseases better understand their care, we, as a community, better understand the lived impact of rare disease on people. A second series of analysis takes place when Advoca looks into its user inputs and extracts data insights. With permission, these insights are collated to produce the essential RWE that is required for advancement of care and treatment for the community as a whole.
In the near future, we’ll be expanding Advoca with a suite of tools to help people better manage their health: document scanning, an Advoca chatbot and additional features designed to give every patient the support they need throughout their care journey. It is easy to see how comprehensive self-advocacy is going to become with the help of safe AI tools for patients.
If you are a person, parent or carer of someone living with a rare disease, you can empower yourself with Advoca for free on your iOS or Android device. If you’re part of a patient advocacy group, you can collectively benefit from Advoca and its RWE. To organise this, please contact us via our website, www.advocahealth.com